What Is Obstructive Sleep Apnea?
Obstructive Sleep Apnea was first described in the literature in the 1960’s. It is the most commonly diagnosed sleep disorder. Other sleep disorders (central, mixed sleep apnea, upper airway resistance syndrome will not be discussed here).
By definition:
- Obstructive sleep apnea (OSA) is the most common type of sleep apnea and is caused by blockage of the upper airway.
- It is characterized by repetitive pauses in breathing during sleep and is usually associated with a reduction in blood oxygen saturation. These pauses in breathing, called "apneas," typically last 20 to 40 seconds per episode.
- The individual with OSA is not always aware of having difficulty breathing, even upon awakening.
- It is recognized as a problem by others witnessing the individual during episodes or is suspected because of its effects on the body.
- OSA is commonly accompanied with snoring.
- Symptoms may be present for years or even decades without identification, during which time the individual may become conditioned to the daytime sleepiness and fatigue associated with significant levels of sleep disturbance.
- Individuals who sleep alone are often unaware of the condition, without a regular bed-partner to notice and make them aware of their symptoms.
In summary, OSA is a severe and potentially life-threatening disease that is often gone unrecognized but should never go untreated! Snoring is often associated with Obstructive sleep apnea and is typically caused by vibration of narrow air passages during sleep. For many people, loud, disruptive snoring is more of a social problem that may strain a relationship. Call 954.771.8772 today to learn more or to schedule your sleep apnea and snoring consultation with Dr. Leslie Sultan!
Difference Between OSA & Sleep Apnea
- All patients with Obstructive Sleep Apnea snore….
- Not all patients who snore have Obstructive Sleep Apnea
- Snoring is considered a condition while OSA is considered a disease
If you suffer from snoring and sleep apnea in Ft Lauderdale, FL, being deprived of oxygen while you sleep can result in poor sleep patterns, daytime tiredness, poor memory, irritability, and strain on the heart and lungs.
Here Are The Facts Regarding The Effects Of OSA On The Body:
- 50% of patients with high blood pressure and heart disease have OSAS
- 77% male and 64% female stroke patients have OSAS
- OSAS may be responsible for 30,000 cardiovascular deaths per year
- OSAS patients are 7 times more likely to be involved in motor vehicle accidents


If you have signs or symptoms of Sleep Apnea, help is available!!!
How Is Sleep Apnea Assessed?
- Do you wake up tired?
- Do you fall asleep easily during the day?
- Does your bed partner notice you stop breathing?
If your score is 9 or above, schedule a consultation to discuss your sleep disorder. Call our office at 954.771.8772.
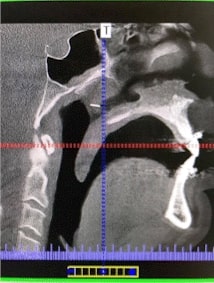
The Initial Evaluation:
In order to diagnose and effectively treat your snoring and sleep apnea in Ft Lauderdale, FL, Dr. Sultan will first evaluate your medical and snoring history and sleeping habits. In addition to the EPWORTH Sleepiness Scale, Dr. Sultan will perform a Cone Beam CT scan (CBCT) to assess your airway anatomy, along with a fiberoptic exam and clinical exam. You may also be sent for a SLEEP STUDY (polysomnogram). This may be done in a sleep center or can be performed in your own home.
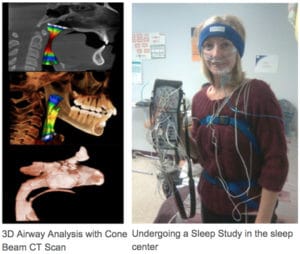
During the sleep study, the severity of sleep apnea is determined by how many times you stop breathing per hour (the Apnea Hypopnea Index or AHI). Obstructive Sleep Apnea is present when the AHI is greater than 5 episodes per hour.
Following your exam and a review of your records, Dr. Sultan will present you with a summary of his findings, and then make recommendations for your treatment.
Note:
It is extremely important that you bring your bed partner to this appointment with you, as they are the ones who witness your sleeping patterns and habits. Also, please bring any X-rays, CT scans, MRI films, Sleep Studies (if applicable), and previous surgical reports. You may request to have the facility that performed these tests forward the films/studies and results to our office. If there is not enough time, please pick them up and bring them with you to your initial consult. Most modern imaging facilities provide their data on a CD for review.
For your convenience, and to reduce your waiting time, we have made our health history form available to you online, which you can fill out prior to coming to your appointment. Please click health history online to fill this form out now.
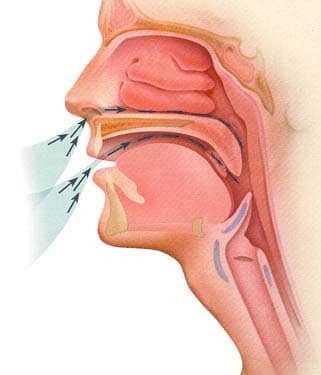
Airway Anatomy:
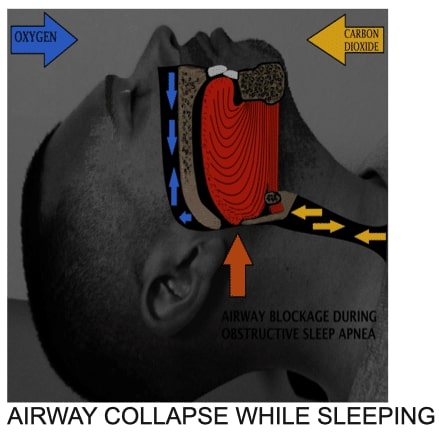
How Obstructive Sleep Apnea affects the upper airway during sleep:
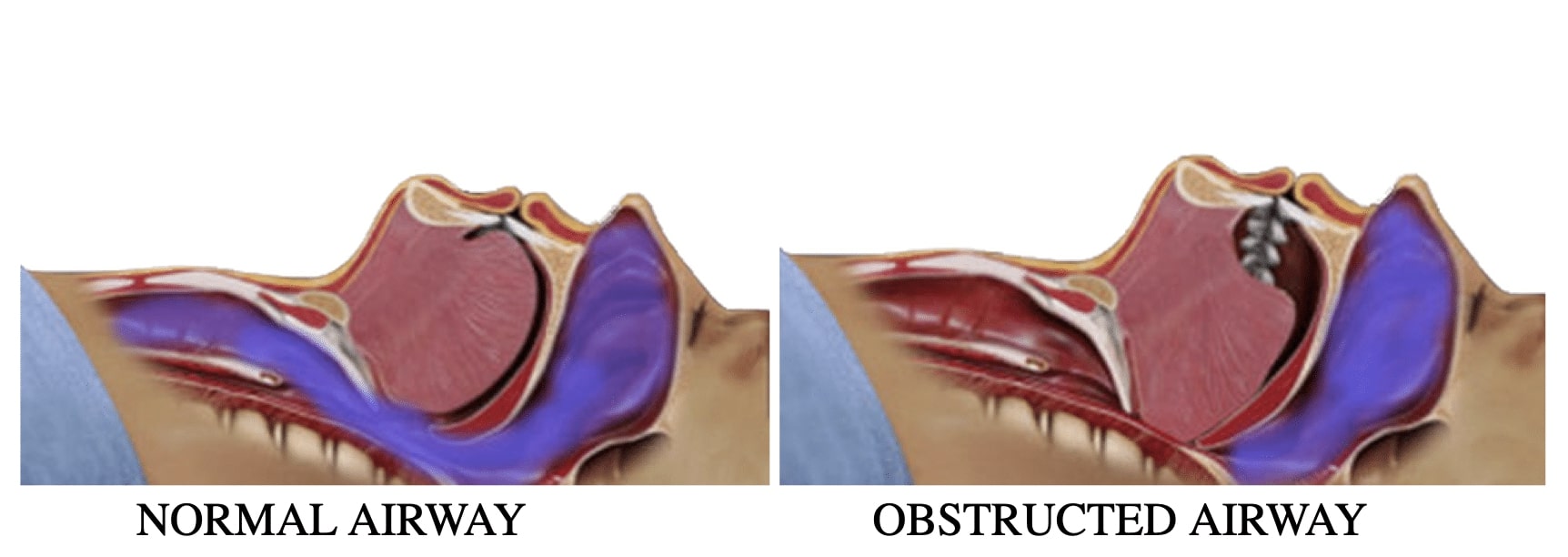
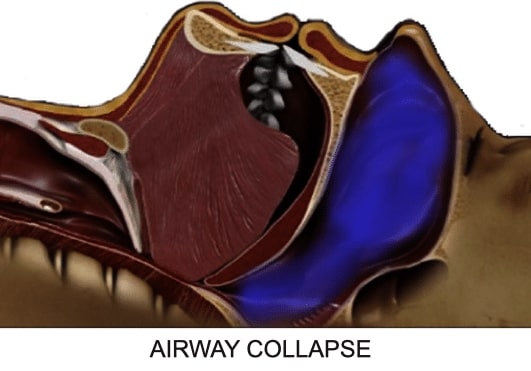
Your Airway collapse during obstructive apnea
The most common areas of blockage are at the level of the:
- Nasopharynx– nasal septum, valves, turbinates, adenoids
- Oropharynx– soft palate/uvula, tonsils
- Hypopharynx– tongue, hyoid bone/neck
- Jaw structure– upper/lower jaw/chin
Although most patients with “common variety snoring” have one central area of blockage, sleep apnea patients often have multiple levels of obstruction.
As the severity of the apnea increases, the magnitude and number of blockages increase.
Not treating all levels of blockage may result in incomplete or ineffective results.
Dr. Sultan prides himself on evaluating the entire spectrum of the upper airway to customize the best treatment for your sleep disorder.
Non-Surgical Options
Consider the main portion of the upper airway as a long, floppy tube with a consistent diameter and circumference ( similar to the plumbing photo below). The tongue, a large mass of muscle, is attached to the back of the chin portion of the lower jaw (mandible). As we lie down to sleep, our mandible falls backward, due to loss of muscle tone, with the bulk of the tongue following along. Unfortunately, evolution has resulted a decrease in overall jaw size. Sleep disorder patients may have excessive soft tissue encircling their airway. Overall, these conditions may lead to a collapse of the upper airway, resulting in hypopnea or apnea.
So it makes sense that any treatment that results in an opening the airway will effectively treat sleep-disordered breathing!
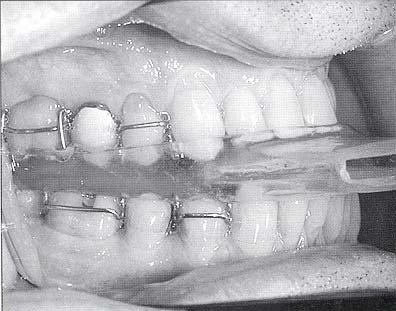
Oral Appliances function by bringing the tongue off the back of the throat during sleep. There are many types on the market (over 50 at last count!). The most common type of appliance repositions the lower jaw forward, bringing the tongue with it. Each appliance is custom made by a dentist who is trained in the technique. Some appliances function by holding the jaw in a set position throughout the night, while others allow the jaw some mobility. Still others function by moving the tongue only.

Here Is The Good And Bad Of Oral Appliance Therapy:
- Advances the lower jaw, opening the airway
- Is diagnostic and therapeutic
- Is successful if tolerated
- Useful for both snoring and some forms of sleep apnea
- Minimal jaw movement throughout sleep
- Potential TMJ problems
- Potential for causing permanent changes in tooth and jaw position, requiring additional treatment
- Less effective as severity of apnea increases
- Approximately 40% of patients using Oral Appliances are NON-COMPLIANT
Continuous Positive Airway Pressure (CPAP) has always and continues to be the gold standard for the treatment of sleep disordered breathing. CPAP functions by allowing the patient to breathe oxygenated air under pressure during sleep. This effectively eliminates passive collapse of the upper airway, removing the symptoms of sleep apnea.
A sleep medicine physician can only prescribe the device. The exact settings are adjusted over time after an initial night in a sleep lab, until all symptoms are minimized. The positive results of CPAP are only good as long as the patient uses the device continuously.
Here is the good and bad of CPAP:
- Very effective in a compliant patient
- Is not effective with nasal congestion. Can cause nasal dryness, sore throat
- Tolerance of mask a problem
- Travel dilemmas
- Percent of non-compliance
- 70% average after 2 years of use
- 46% actual compliance for regular use (4 hours per night on 70% days)
- 6% actual compliance for adequate use (7 hours use for > 70% days)
When Is Surgery Considered For Sleep Apnea?
The goals for the treatment of sleep disordered breathing are based on the expectations of each patient’s quality of life. It would be great if every doctor could promise 100% success in each treatment provided. Unfortunately, this is not the case.
Treatment success is therefore relative, and based on each patient’s symptoms and response to treatment. If a patient with a loud “roar of a snore” is reduced to a low hum, that may be considered a successful outcome. If a 50% or greater reduction in a patient’s Apnea Hypopea Index can be achieved, the same is true. However, if a patient cannot tolerate the treatment (non-compliance), not even the most favorable results can be maintained.
Therefore, surgery for the treatment of Sleep Disorder Breathing is indicated for those patients:
- who cannot/will not tolerate the use of non-surgical modalities (appliance, CPAP)
- as an adjunct to improve the outcome of non-surgical therapy
- failure of complaint patients to achieve relief of symptoms with non-surgical therapy alone
Your Surgical Options
As you have read, snoring and obstructive sleep apnea are caused by blockages in the airway. Thankfully, there are a number of surgical procedures available that can help remove these blockages permanently.
To obtain the proper result, each area of blockage must be identified and treated individually. Based on the severity of the disease, a combination of procedures may be recommended. Depending on the results of therapy, additional procedures may be indicated. A follow-up sleep study is generally performed a few months after surgery, to effectively gauge reduction in symptoms.
Therefore, treatments concentrate on either reducing, stiffening, repositioning, or removing both the soft and hard tissue that is blocking the airway.
Below are some of the most common procedures recommended by Dr. Sultan:
Nasal Airway Obstruction
Nasal airway obstruction can be uncomfortable and annoying. Blocked nasal passages force you to breathe through your mouth, making simple, everyday activities such as eating, speaking, and sleeping more difficult. Many patients with Obstructive Sleep Apnea have some degree of nasal obstruction.
What causes nasal obstruction?
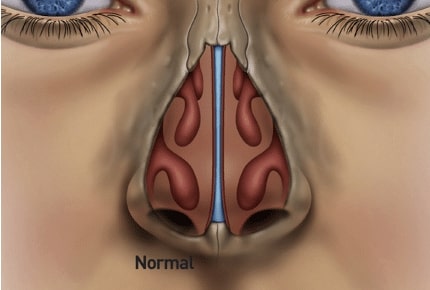
Three main structures contribute to a blockage within the nose:
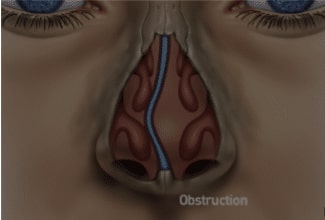
1. The nasal septum, a piece of cartilage dividing the two sides of the internal nose, can be deformed, causing physical blockage to airflow.
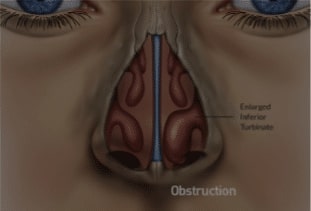
2. Nasal turbinates facilitate the conduction, filtration, heating, and humidification of the air we breathe. Allergies or environmental irritants (such as smoke or household chemicals) are the most common cause of irritation, inflammation, and enlargement of turbinates, resulting in blocked nasal passages. Additional causes of turbinate enlargement include anatomical causes (such as a deviated septum) and hormonal changes (such as those that occur during pregnancy). Turbinate size can also fluctuate throughout the day, especially depending on head position (i.e. standing up versus lying down).
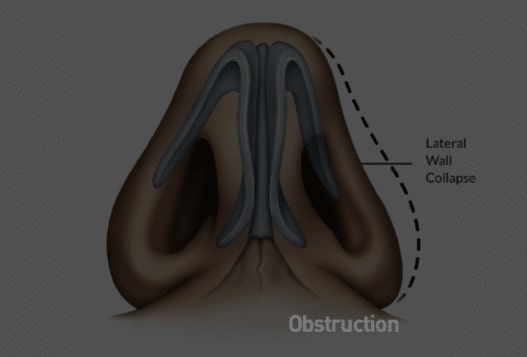
3. Due to excessive negative pressures caused by nasal obstruction, the cartilaginous lateral nasal walls can collapse inward.
**Each of these structures contribute to difficulty in nasal breathing. In addition, patients already using CPAP can have difficulty tolerating their device due to this blockage.
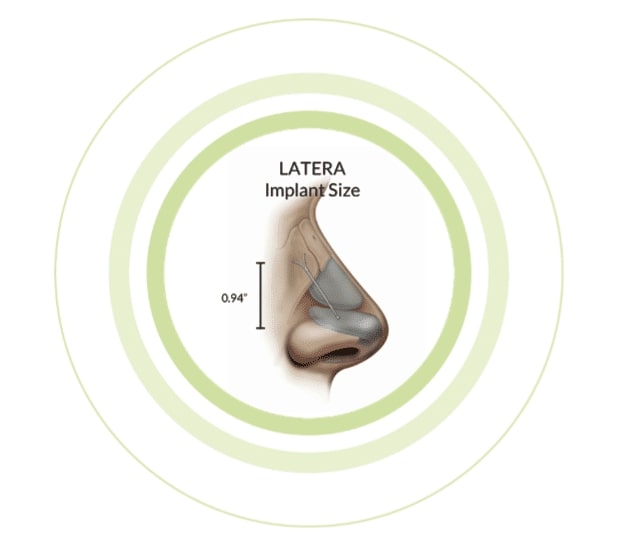
LATERA®
THE SOLUTION TO LATERAL NASAL VALVE COLLAPSE
The Latera® procedure involves the insertion of a thin, resorbable implant into the sidewalls/lateral nasal walls, allowing increased support. This results in decreased nasal airway resistance, and increased airflow. It can be done as a standalone procedure or combined with other nasal procedures to open this area of the upper airway.
Treatment Options For Nasal Airway Obstruction
Traditional medical therapy, including allergen/irritant avoidance and/or use of nasal medications, may be sufficient to address turbinate enlargement. In some cases, however, turbinate enlargement is unresponsive to medical management.
Coblation® is an advanced technology that quickly removes and shrinks soft tissue inside the turbinates using gentle radiofrequency energy and natural saline to alleviate nasal obstruction in patients. Coblation is not a heat-driven process. As a result, surrounding healthy tissue is preserved. This quick outpatient procedure takes less than 10 minutes. Patients typically return home shortly after the procedure, and can experience a 50% reduction in nasal airway obstruction within one week.
Coblation (Radiofrequency Volumetric Reduction)
RadioFrequency(RF) is a technique used to shrink or reduce the size and bulk of these tissues. This process also results in a stiffening of these tissues, preventing them from vibration as air passes through.
Coblation® is an advanced technology that combines gentle radiofrequency energy with a natural salt solution, which quickly and safely reduces tissue size and bulk. Traditional procedures may cause excessive bleeding or use high levels of heat that may cause damage surrounding healthy tissue. Coblation does not cause heating or burning, which leaves the healthy tissue surrounding the target tissue unaffected.
The Coblation Procedure uses a temperature-controlled radio frequency to reduce and tighten the tissues of the nose, palate/uvula, tongue, and tonsils. The treated area is heated and slowly absorbed by the body over a 3 to 8 week period. It is relatively painless, and it is an effective treatment for snoring, nasal obstruction, and mild sleep apnea.
Snoring is due to the vibration of the soft tissues in the airway. Although most people are familiar with the effects of a large, floppy soft palate, other tissues may be involved. They include nasal turbinates in the nasal airway, the tongue base, and tonsils. The uvula (a floppy muscle attached to the base of the soft palate) may also be a culprit.
Some patients may be familiar with Somnoplasty, which also uses radiofrequency energy to volumetrically reduce soft tissue size. We have found the Coblation technique to offer superior results with fewer complications.
The Evolution Palatal Surgery
Is It Effective?
Palatal Surgery involves the reduction, repositioning, and in some cases, removal of loose, floppy tissue at the back and top of the mouth. Since most snoring involves a palatal component, surgery is very helpful.
However, recent evidence-based studies have shown that palatal surgery alone is not an effective treatment for sleep apnea. The best results are found when palatal surgery is combined with other procedures for opening the upper airway.
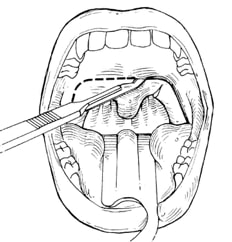
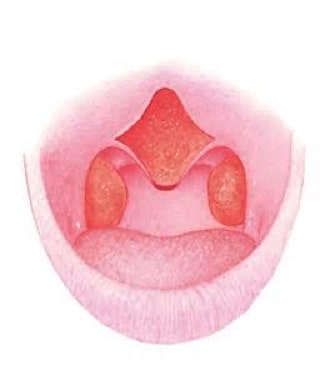
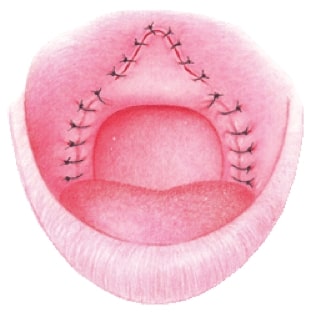
UPPP/LAUP
The traditional approach to surgically treating excessive palatal tissue is the uvulopalatopharyngoplasty (UPPP). Historically, it is reserved for patients with obstructive apnea. A portion of the soft palate, along with the tonsils and uvula, are removed in order to open the airway. The procedure is done under general anesthesia in the hospital, and commonly requires a prolonged recovery. Because the palatal musculature is altered and the palate is shortened, the procedure has an increased risk of difficulties in swallowing and fluids going through the nose while drinking (nasal reflux). It has been described as a painful procedure. Unfortunately, the success rates in the literature do not exceed 50% when performed alone. In hopes of reducing postoperative complications, the carbon dioxide laser was used to carry out a modification of the UPPP (Laser Assisted Uvulo Palatoplasty). The LAUP was performed for treatment of both apnea and snoring. The postoperative pain and variable results led to the development of more refined, less invasive palatal procedures, which in many cases yield equivalent or better results than the UPPP.
LAUP is not typically performed for current treatment of Snoring/Obstructive Sleep Apnea
Traditional Uvuloalatalphayngoplasty (UPPP)
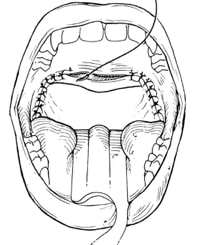
Uvulopalatal Flap
A modification of the UPPP is the Uvulo-Palatal Flap (UPF). This technique involves the repositioning of the lower portion of the soft palate without altering or removing the palatal muscles. The result is a less postoperative pain, significantly reduced the risk of nasal reflux, and a speedier recovery.
Pre and postoperative Uvulopalatal Flap
Palatal Suspension Suturing Techniques
An alternative to removing palatal tissue, this minimally invasive technique involves placement of non-dissolving sutures beneath the palatal surface tissue to suspend and advance the lateral and inferior portions of the soft palate. This “palatal facelift” is effective in expanding and reshaping the palatal opening, without removal of palatal musculature, so full palatal function is intact.
Combination UPF/Coblation
Coblation® technology can be used independently to shrink the palate for those patients who snore and have mild apnea. The procedure is performed under a local anesthetic in the office. Postoperative discomfort is minimal, and results are seen within 3 to 6 weeks.
Coblation can also assist in the UPF to reduce pain and bleeding. A recently developed variation involving the removal/repositioning of tissue (Coblation Assisted Uvulo Palatoplasty) can be performed with very promising results.
Tongue Suspension & Hyoid Advancement
The Key To Treating Advanced Airway Obstruction
The base of tongue is a large, floppy tissue that poses a significant bottleneck in air passing through the vocal cords into the lungs. The hyoid bone, a floating bone found beneath the tongue, functions along with the tongue to control swallowing, breathing and jaw movements.
Most importantly, both the tongue and the hyoid bone have muscle groups attaching to the chin area in the mandible/lower jaw.
In obstructive sleep apnea, as the lower jaw falls back as we lie down, the loose musculature attaching the jaw to the tongue and hyoid relapse, causing a blockage of the airway.
This area, known as the hypopharyngeal airway, can be the most significant location of obstruction in OSA.
Untreated, it can perpetuate sleep apnea. If unaddressed during surgical treatment planning, it can significantly reduce the success of surgical outcome.
Like the palate, there are many different traditional methods to treat the tongue base and hyoid by either reducing, repositioning, or eliminating tissue.
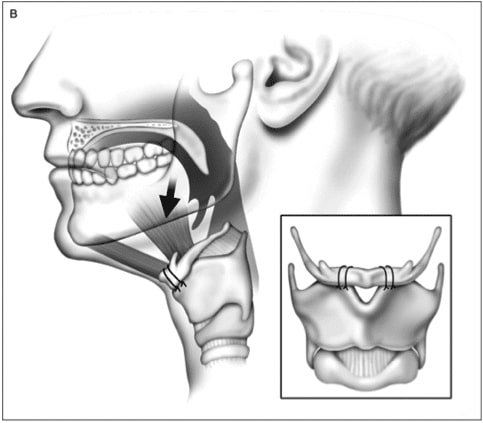
The early, traditional methods of addressing this area were to pulling the muscles of the tongue through a bony window in the chin, or suturing the hyoid bone to the throat cartilage.
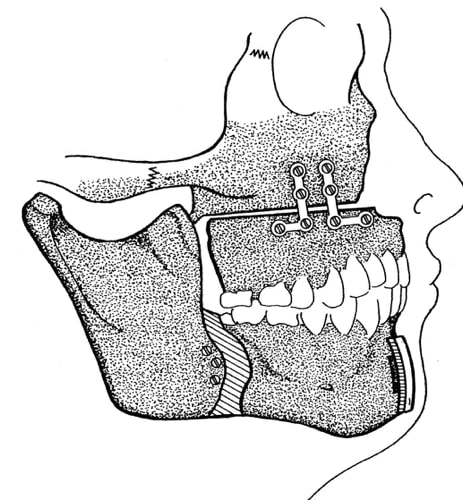
The Airlift™ Technique
Studies have shown that the combination of suspending the tongue base muscles along with advancing the position of the free floating hyoid, increases the success of reconfiguring the lowest, and most important part of the obstructed airway.
The AIRLIFT™ procedure is less invasive than traditional methods with very favorable results. The technique involves one or two small incisions in beneath the chin/neck. Small titanium screws are placed below the chin. Non-dissolving sutures are then threaded around the hyoid bone and within the base of the tongue and then tightened. The procedure is very well tolerated, the results are long term, adjustable and reversible. The procedure is used for all levels of obstructive apnea, but best suited for moderate to severe patients.
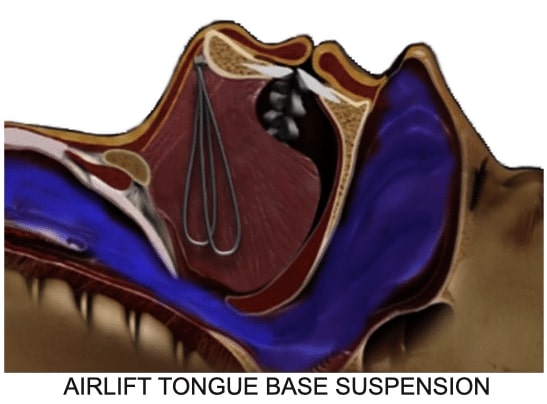
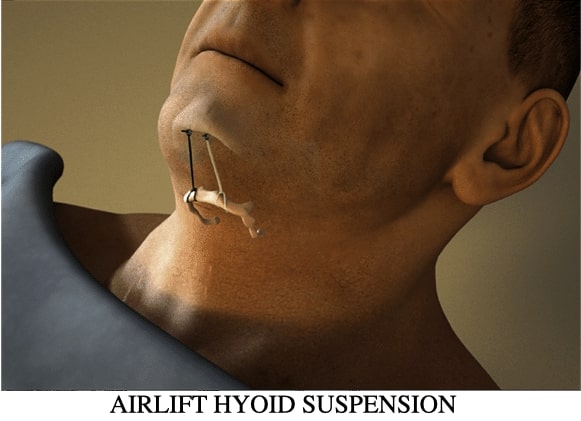
DR. SULTAN IS ONE OF THE VERY FEW SURGEONS IN ALL OF SOUTH FLORIDA TRAINED AND EXPERIENCED IN PERFORMING THE AIRLIFT™ PROCEDURE!
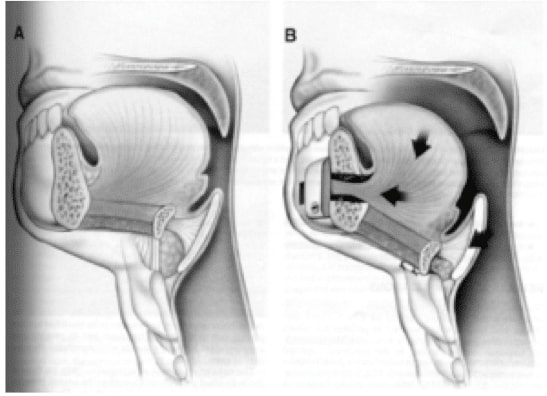
Jaw Repositioning Surgery
Out of all the surgical procedures available for treating obstructive sleep apnea, advancement of the jaw structure provides the best overall outcomes. Once considered the “last resort”, jaw repositioning was only considered when “less invasive procedures” were ineffective in sufficiently improving symptoms. Currently, there is sufficient evidence to support these techniques early on in treatment sequencing, or as a primary, “stand alone” procedure.
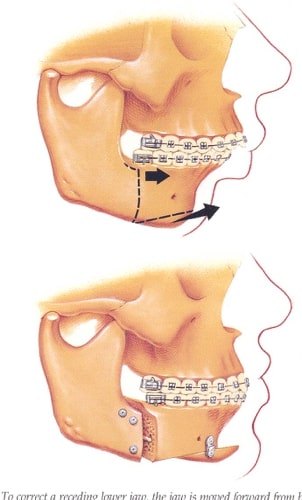
Why Does It Work?
Morphologically, we see patients with obstructive apnea fall into two basic categories: those with excessive soft tissue blocking the airway, or with a deficiency or setback in the jaw structure. These bony deficiencies present as an “underbite,” or a flat facial profile. These patients may have previously undergone orthodontic therapy, many with the removal of teeth, in order to correct the bite, but overlooking the functional deficit causing airway obstruction.
As the tongue musculature attaches to the back part of the lower jaw, advancing that bone will also advance, and suspend the tongue. This is the premise behind the use of an oral appliance. In fact, an oral appliance can be used as a diagnostic tool in planning for jaw repositioning surgery. Similarly, advancing the upper jaw will open the restriction of the soft palate musculature off the back of the throat.
How Is It Performed?
These procedures are performed by surgeons skilled in both orthognathic and sleep apnea surgery. The planning and mechanics of the procedure are unique, in order to maximize airway opening as well as facial aesthetics. Depending on the jaw and bite relationship, surgery may be done in coordination with orthodontics. Surgery can be performed only in one jaw, or by bringing both jaws together as a unit.

Planning of the surgery is enhanced by state of the art, computer-guided planning. By using titanium plates and screws, the jaws are not wired shut following surgery. Patients undergoing jaw advancement surgery routinely experience immediate, long-lasting relief, and many times, a cure from obstructive sleep apnea!
Treatment Sequencing / It All Together
Depending on the severity apnea and the sites of airway blockages, some patients may not require surgery, but others might. Other patients may require a combination of both medical and surgical management. Furthermore, some patients may require more than one surgical treatment to achieve the best results.
For Those Patients Who Snore Without Evidence Of Sleep Apnea:
- Blockage is typically in one anatomical area, usually the palate or nasal areas
- Non-surgical management may effective (oral appliance)
- Lesser invasive surgical options that REDUCE OR REPOSITION TISSUE may be effective
- Coblation
- Palatoplasty/Palatal Flap
- If surgical procedures are ineffective, patients should consider a sleep study to rule out obstructive sleep apnea
For Patients Diagnosed With Mild Obstructive Apnea:
- Blockage may be at more than one site (nasal/palatal or palatal/tongue)
- Non-surgical methods should be considered first (CPAP, oral appliance)
- Surgery should be directed towards each obstruction site to REDUCE OR REPOSITION TISSUE:
- PALATE – Palatoplasty with Coblation/Suspension Suturing
- NASAL – Coblation Turbinate reduction, nasal valve repair, septoplasty
- TONGUE/HYOID- AIRLIFT procedure
- JAW DEFICENCY – consider Jaw repositioning
- Follow up sleep study is recommended 3 to 6 months following treatment
- Consider jaw advancement surgery if the above recommendations fail to achieve success in relieving symptoms
For Those Patients With Moderate To Severe Apnea:
- Blockage is at two or more levels
- CPAP should be considered at evaluated.
- Oral appliance therapy may be regarded as diagnostic for success of jaw repositioning surgery, or to decrease the need for CPAP
- Surgery is directed towards each level of obstruction to REDUCE, REPOSITION, OR REMOVE TISSUE
- PALATE– palatoplasty
- NASAL– turbinate reduction/removal
- TONSILLAR– reduction/removal
- TONGUE– AIRLIFT
- HYOID– AIRLIFT
- MAXILLOMANDIBULAR ADVANCEMENT can be considered as a first line procedure, or performed if multilevel airway techniques fail to achieve success
Closing Pearls
- Snoring is a condition caused by a partial blockage of the airway
- In this instance medical insurance does not offer coverage for this condition
- Although not all snorers have apnea, all patients with sleep apnea snore
- Sleep apnea is a serious disease and should be respected for its impact on overall health
- Obstructive sleep apnea is a disease caused by airway obstruction at multiple locations
- Failure to address and treat each level of obstruction may result in a poor surgical outcome
If you’re one of the many people who can’t stop snoring, Dr. Sultan, your snoring & sleep apnea surgeon, can help! Remember, the overall goal of surgical treatment is to help you and your partner have a future full of restful nights, without you ever having to be inconvenienced by or depend on CPAP or appliances again.
You can be sure that Dr. Sultan will always keep your comfort, convenience, and what is most cost-effective for you in mind when planning your treatment.