TEMPOROMANDIBULAR DISORDERS

TMD, or Temporomandibular Joint Disorder, is a term which covers a wide range of painful oral and facial symptoms involving the jaw joint (TMJ) and the surrounding facial muscles. These symptoms may include pain in front of the ear, joint noises, headache, limited mouth opening, jaw locking, and change in bite. As TMD progresses, it can cause symptoms affecting one’s daily quality of life. Fortunately, at the Sultan Center for Oral Facial Surgery in Ft Lauderdale, Dr. Sultan can provide both non-surgical and surgical options to treat this condition.
WHAT ARE THE CAUSES OF A TEMPOROMANDIBULAR DISORDER?
In most cases, TMD involves a combination of disorder of the joint, soft tissues surrounding the joint and psychosocial factors (stress, bruxism). The most common causes of TMD include:
- Trauma (fracture, motor vehicle injury, occupational)
- Pathology (tumors of the jaw joint)
- Arthritis (degenerative, rheumatoid)
- Bony resorption
- Skeletal/dentofacial deformity
- Malocclusion
- Internal derangements (disorder of the joint structure/function)
- Medical conditions
- Stress
- Bruxism
- Obstructive sleep apnea
How is a Temporomandibular Disorder Diagnosed?
Prior to your visit with Dr. Sultan, a thorough questionnaire describing your symptoms, events leading up to the condition, and past treatments will be completed. During your visit, your condition, medical/dental history will be discussed in detail. Following a clinical evaluation, a Cone Beam CT scan (CBCT) is taken to assess the bony anatomy of your facial structures. Once an initial diagnosis is made, additional imaging studies may be ordered (MRI, bone scan). For patients with a sleep disorder, a sleep study will be ordered. If your condition involves a jaw deformity/malocclusion, 3D scans of your bite are required. Consultations from other specialists may be recommended to aid in diagnosis and treatment.

What Are the Goals of Treating Tmd?
When treating TMD, Dr. Sultan will carefully explain the concept of:
Treat to cure vs. Treat to manage
With this in mind, the ultimate goals in properly addressing your condition are:
- Accurate diagnosis
- Evidence-based treatment modalities
- Setting realistic goals for treatment
- Providing long-term maintenance
- Improving quality of life

UNDERSTANDING THE PATHOPHYSIOLOGY OF TMD
TMD involves a close relationship between:
- Your joints
- Muscle groups and posture of the jaw, head, and neck
- Jaw & skeletal position
- Bite relationship
- Airway
In order to best understand the different procedures available, it is important to appreciate how the TMJ functions and its progression of disease.
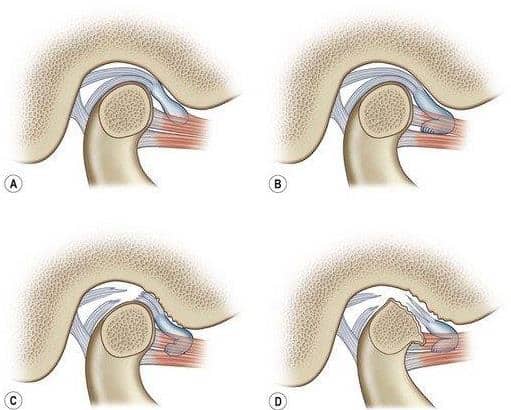
The TMJ, like other joints in the body, can be described as a ball-and-socket mechanism. Separating the bony portions is a cartilaginous disc (meniscus). The meniscus is held in place by a series of ligaments. The meniscus has no nerves or blood vessels, the ligaments do. Above and below the meniscus are pockets of fluid providing nutrition and lubrication (synovial pockets). The meniscus should remain and freely move along with the condyle (ball portion) of the joint in all movements including rotation, translation, lateral and protrusive movements.
In general, any time a joint is overloaded or stressed, it begins to break down. This condition is known as an internal derangement. In the TMJ, the progression of disease is described in five stages (Wilkes 1-5):
- Early disc displacement: No pain, no limited opening, early click
- Late disc displacement with reduction: Pain, progressive limited opening, occasional locking
- Complete disc displacement: Jaw locked, absence of noises, restricted mobility
- Non-reducing deformed disc: Perforation, mild improvement in opening, pain, no arthritic changes
- Non-reducing deformed disc: Limited joint space, bone to bone, crepitation, limited function, skeletal changes, end stage Chronic inflammation of the joint structures can affect and cause symptoms involving the surrounding muscles as well as the ear.
- As degenerative joint changes develop, changes in jaw position can result in bite deformities.
- As the lower jaw rotates back, the posterior airway can become diminished resulting in an obstructive sleep disorder.
An important part of your treatment is proper diagnosis, and recommending appropriate treatment modalities based on all these areas of concern.
NON-SURGICAL TREATMENT OPTIONS FOR TMD
When diagnosed and treated properly, the majority of patients will obtain relief from non-surgical and REVERSIBLE modalities. These include:
- Limitation of mouth opening
- Diet modification
- Moist heat
- Medications (anti-inflammatories, muscle relaxants)
- Stress management
- ORTHOTIC device
- Soft tissue management/physical therapy
If an orthotic device is recommended, it should be custom, made out of hard material and allow your jaw to be supported and move freely.
When these non-invasive treatments fail to relieve the symptoms of TMD, and there is documented pathology in the TMJ itself, surgery should be considered.

WHAT IS AN ORTHOTIC?
An orthotic is defined as “a medical device (such as a brace or splint) for supporting, immobilizing, or treating muscles, joints, or skeletal parts which are weak, ineffective, deformed, or injured.”
For TMD, an orthotic device ideally is a patient-specific custom device made to provide support for the joints, teeth and surrounding muscles.
The process of designing and fabricating an orthotic begins with obtaining digital records of your teeth and bite relationship.
The orthotic should be designed to provide full coverage of all your teeth, and allow for proper thickness and trajectory for all jaw movements.
The orthotic is inserted and adjusted as often as necessary to provide patient comfort when wearing the device.
The orthotic is both diagnostic and therapeutic. It is an important part of therapy, whether it be with or without surgery.
We normally recommend our patients wear their orthotic as much as possible, except for during eating and oral hygiene. Once their condition has stabilized, the use of the device is slowly weaned.
Oral orthotics are designed based on each particular patient. The goals of each device are:
- To provide support for the joints
- To control, reduce or eliminate clenching/grinding
- Reduce inflammation in the joints and surrounding muscles
- Allow the jaw to “find” it’s most comfortable position
What is a splint/niteguard/biteguard?
Unfortunately, patients and dentists use these terms interchangeably, but they are not the same. They each are made differently and have a different purpose. They are different from orthotics in their design and use.
ASSESSING THE EFFECTS OF NON-SURGICAL THERAPY
Fortunately, most patients with TMD respond favorably to non-surgical therapy. There are three treatment paths that we see:
- Gradual improvement over time until patient is symptom free
- Improvement until a plateau is reached where symptoms remain unchanged.
- No change or increase in symptoms over time.
For those patients having documented disease in their joints or surrounding structures, and desire an improvement in their quality of life should consider surgical options.
TMJ SURGERY & TMJ REPLACEMENT
The Art and The Science
WHAT ARE INDICATIONS FOR TMJ SURGERY?
Conditions in which surgery is considered as a primary approach are:
- Hard and soft tissue deformities of the TMJ
- Ankylosis (bone/soft tissue fusion of the TMJ)
- Traumatic injuries of the TMJ (severe)
- Tumors of the TMJ
Those conditions in which surgery should be considered secondary along with non-surgical therapy are:
- Arthritis (degenerative/rheumatoid)
- Internal derangements (Grade 2,3,4,5)
- Condylar resorption (idiopathic, traumatic, congenital)
- Chronic dislocation
- Associated skeletal/dentofacial deformities
WHAT ARE THE GOALS OF TMJ SURGERY?
Dr. Sultan will have a detailed discussion regarding what each patient’s individual goals are from their recommended procedure, including:
- Pain reduction
- Improved mouth opening
- Return to normal diet
- Correction of jaw/bite relationship
- Improved airway/breathing
- Reduce/eliminate need for orthotic
Dr. Sultan strongly believes in the use of evidence-based surgical procedures:
- Develop the proper diagnosis
- Perform the surgical procedure that has been shown in the literature for the best long term results
Patient’s play an important role in the success of their procedure by strictly following their postoperative instructions.
What People Say About Us!
I had the privilege of being treated by Dr. Sultan, the best maxillofacial surgeon I could have ever hoped for. Dr. Sultan’s expertise, compassion, and skill were truly exceptional. From the moment I walked into his office, I felt at ease. Dr. Sultan took the time to thoroughly explain my condition, the treatment options, and what to expect. Throughout the entire process, I felt confident in Dr. Sultan’s abilities and Staff. The recovery was far smoother than I had anticipated, thanks to Dr. Sultan’s meticulous care. I can now say that my quality of life has drastically improved. I can't recommend Dr. Sultan highly enough for anyone seeking top-notch maxillofacial care.
Click here to read more reviews.
Dial 954.771.8772 to reach our Fort Lauderdale office, and our staff will help you set up your TMJ consultation.
TMJ SURGICAL OPTIONS
JOINT INJECTION
JOINT INJECTION
- Although not a true surgical procedure, an injection in or around the joint capsule can be both diagnostic and therapeutic. A mixture of local anesthetic and steroid are placed in order to reduce pain and inflammation. They are indicated for an acutely inflamed joint, or to differentiate the true cause of symptoms.
ARTHROCENTESIS
- An office based procedure involving the irrigation of the joint using small needles, usually performed under sedation.
- Additional administration of either joint lubrication or stem cell /PRGF products improve and prolong joint mobility.
- Reserved for patients with acute/chronic joint inflammation, acute closed lock or sometimes following other joint surgeries
ARTHROSCOPY
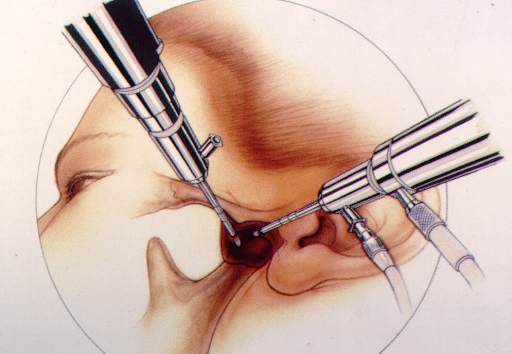
- Can be either diagnostic or therapeutic
- It is normally performed as an outpatient under sedation or general anesthesia.
- The approach involves making 2 or 3 inconspicuous puncture sites in front of the ear.
- The joint can be flushed with visco-lubricant/stem cell/PRGF when indicated.
- Clinical conditions that respond well to this procedure include a chronically displaced disk with a locked joint/closed lock.
- It can also be therapeutic for a patient with inflammatory arthritis.
- The goals of this procedure are to remove inflammatory tissue from the joint, free up scar tissue, and increase joint mobility.
ARTHROPLASTY
- Classic, open surgical treatment for disc displacement. It is performed as an outpatient in the hospital with general anesthesia.
- A small incision is placed cosmetically through a crease in front of the ear. This incision becomes inconspicuous following healing.
- The main requirement for this approach includes management of the disc/meniscus with a healthy mandibular condyle (ball portion).
- If the disk is salvageable, it can be repositioned, and then secured to the condyle. An anchor is inserted into the bone, and the meniscus is secured to the functioning portion of the condyle with sutures. This is a discopexy.
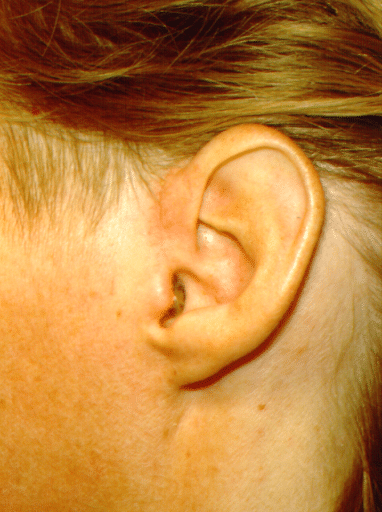
Esthetic incision for arthroplasty
- The ligaments of the joint can also be tightened if necessary. Also, prominent bone preventing normal condyle movement can be reduced (eminectomy).
- Visco-supplementation is placed into the joint space.
- This procedure is the treatment of choice for patients with Wilkes 2 and 3 disease.
- If the meniscus is beyond repair (Wilkes 4), it must be removed (meniscectomy). A temporary plastic spacer is placed, and is removed a few weeks later in the office.
Dr. Sultan has made innovative modifications to the classical procedure to dramatically improve the success of this procedure. Dr. Sultan is one of the very few maxillofacial surgeons in Florida performing this procedure.
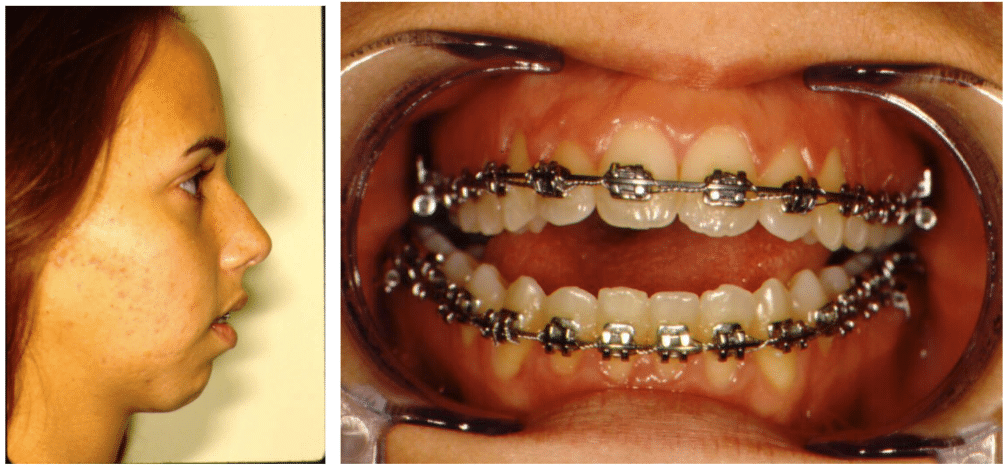
TMD AND ORTHOGNATHIC SURGERY
- As a general rule, the joints should be healthy prior to jaw repositioning (orthognathic surgery)
- If TMD begins or develops during the course of pre-surgical orthodontics, non-surgical and/or TMJ surgery may be necessary. Active tooth movement should be stopped until the TMD has subsided/resolved.
- The presence of untreated internal derangements increases the chance of relapse after orthognathic surgery by as much as 25%
- Treatment sequencing in cases may require non-surgical and/or surgical TMD treatment prior to jaw surgery
- In the presence of end stage joint disease (Wilkes 5) total joint replacement (TJR) may be required along with orthognathic surgery.
TOTAL JOINT REPLACEMENT (TJR)
For those patients with end stage joint disease, removal and replacement of all the joint structures may be necessary.
Indications for this type of surgery include:
- Symptomatic Stage 5 internal derangement
- Inflammatory or rheumatoid arthritis that has not responded to other therapies
- If the tissues of the joint fuse (ankylosis) causing loss of motion in the joint, resulting in inability to open the mouth properly
- If bite changes and/or facial appearance has changed as a result of a TMJ problem (condylar resorption)
- If previous attempts at surgery by opening the joint have failed to resolve the problem (multiply operated patient)
- Loss of normal anatomy of the joint due to trauma or pathology of the TMJ
Depending on the patient’s age and condition, this form of TMJ treatment can be performed with either natural or artificial materials.
For an actively growing patient, the use of a patient’s own rib is preferred.
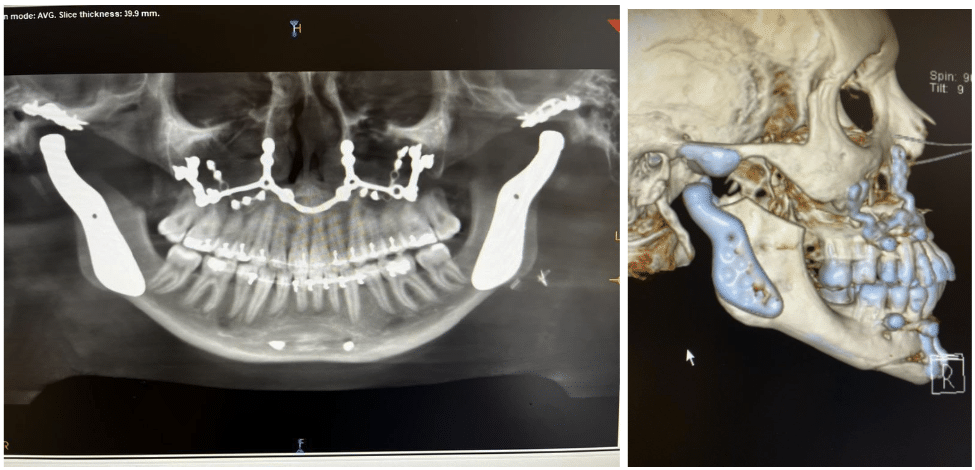
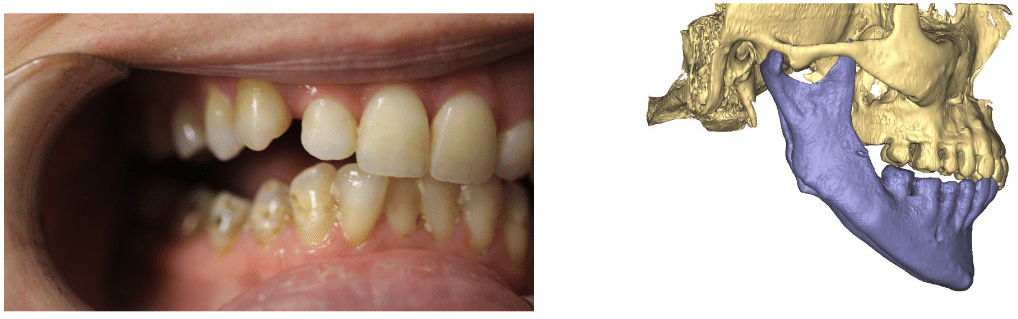
Correcting condylar resorption/open bite with rib graft
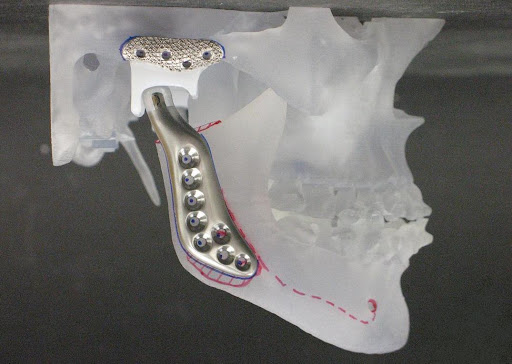
For an adult or when active jaw growth is complete, we prefer the use of a metallic joint replacement, which has been shown to have a high rate of long term success with low risk or need for revision.
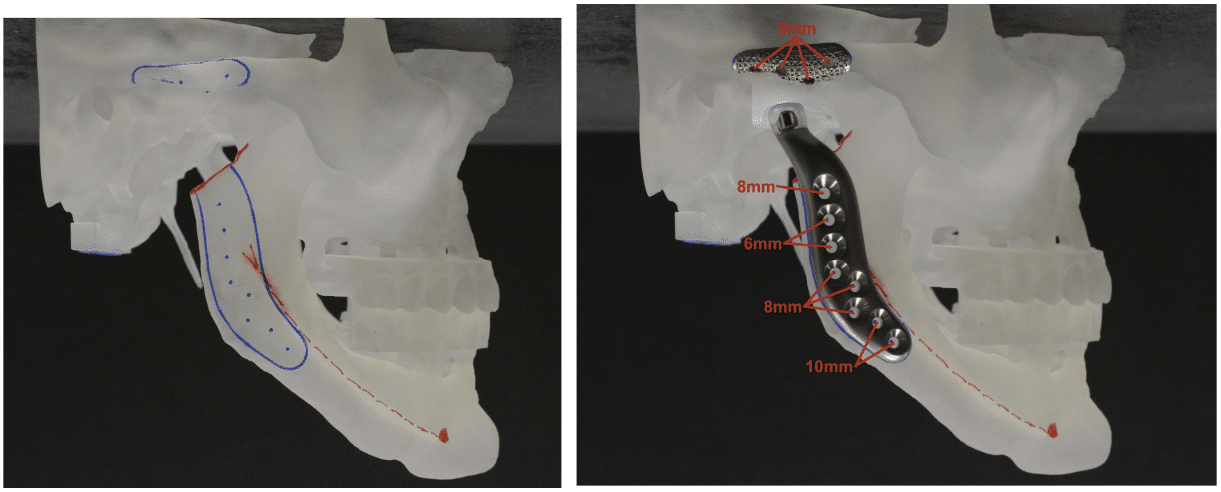
The current replacement systems are either stock (pre-made, off the shelf)) or patient specific (custom).
Dr. Sultan has been performing TJR surgery since 1990 , currently utilizing the Stryker TMJ Concepts prosthesis. He is one of the few and most experienced joint replacement surgeons in the southeast US.
Like other joint replacement systems in other bones of the body, the joint has a metal/plastic articulation. The metal components are titanium and chrome cobalt - an all titanium version is also available.
Please advise Dr. Sultan if you have a documented metal allergy!!
THE TJR PROCESS
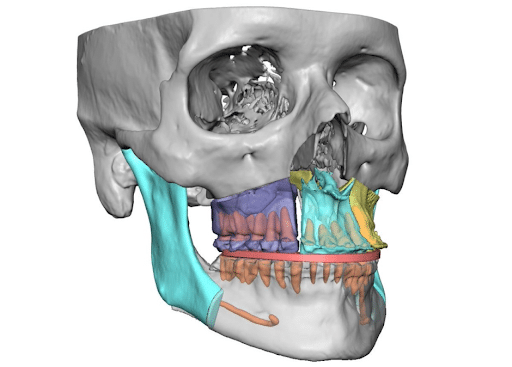
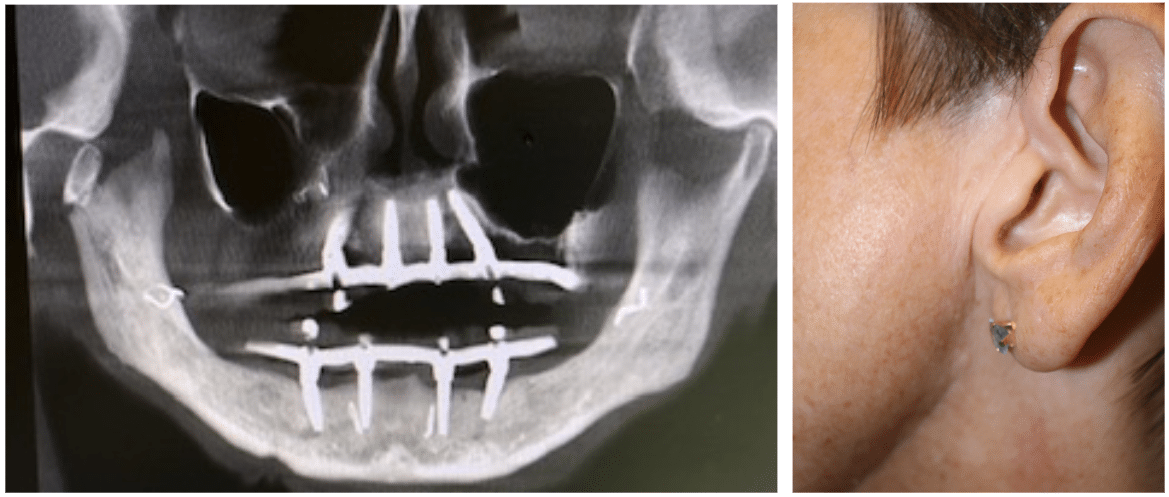
Patient specific joint prostheses are custom made to each patient’s anatomy. The process begins by obtaining digital diagnostic records (CT scan, tooth/jaw scans). Data is uploaded to our modeling engineer who develops a virtual surgical plan for designing the bone removal and replacement. If there is associated malocclusion or jaw deformity, additional diagnostic planning will be required to reposition the upper jaw/lower jaw/chin (orthognathic surgery). Once the virtual plan is approved, the manufacturing process takes about 3 months to complete.
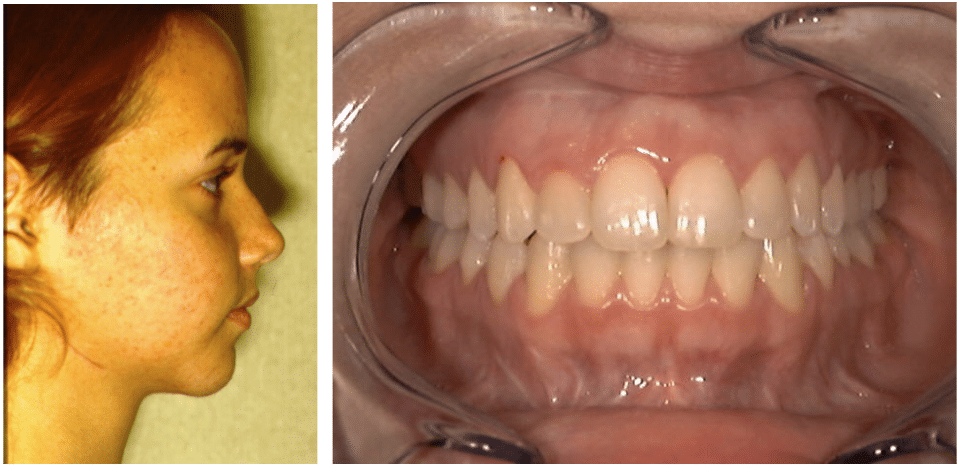
TJR CASE STUDY
Patient with traumatic injury to TMJ
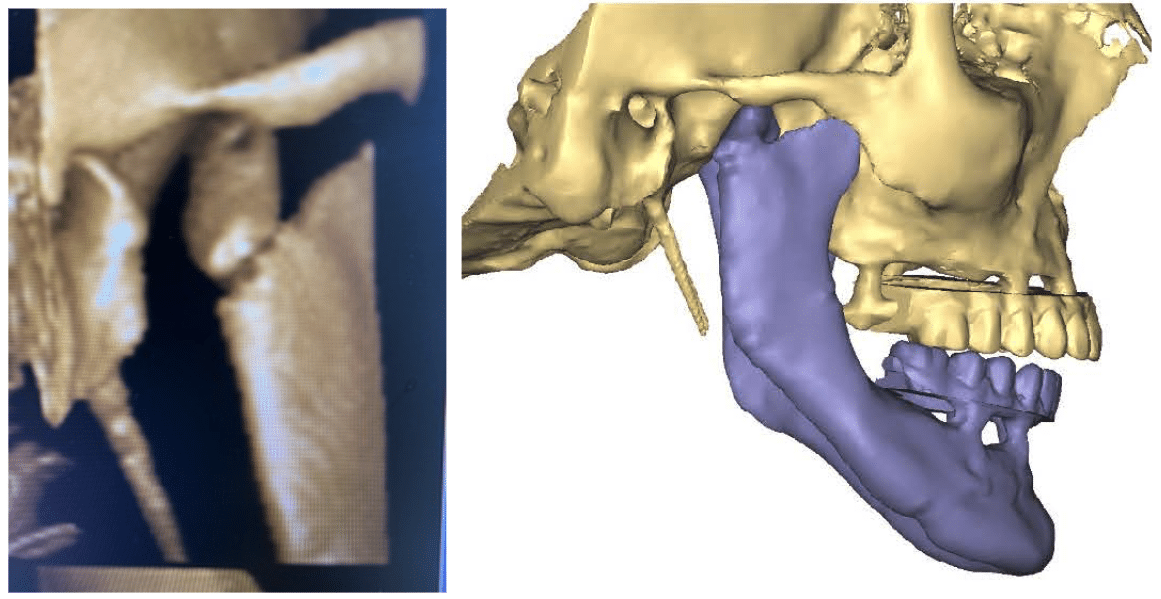
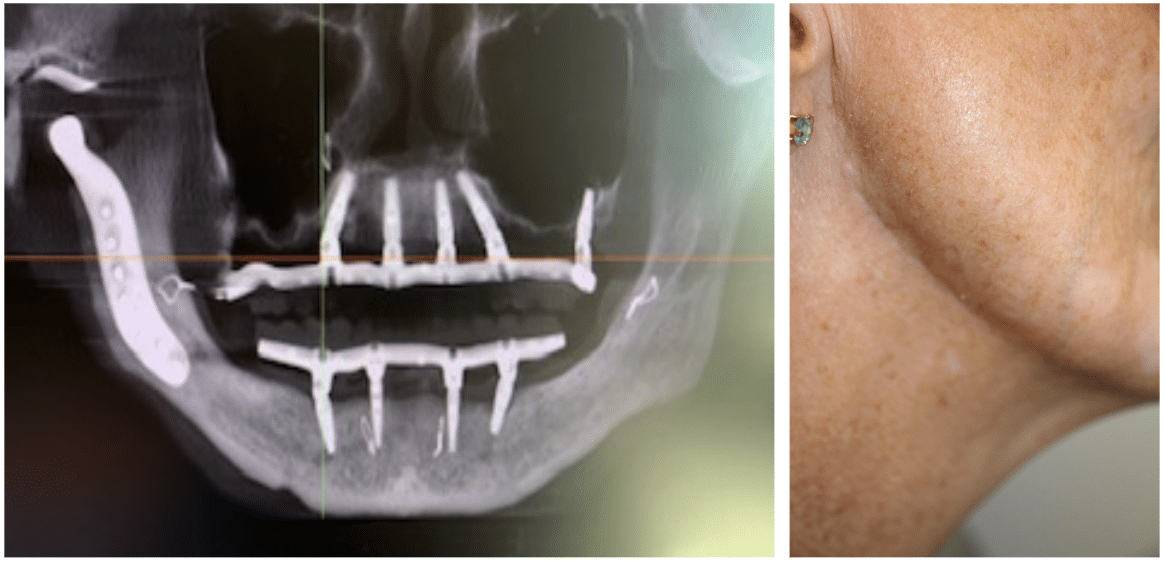
For certain conditions, e.g.ankylosis, joint replacement may be done in (2) procedures.
THE TJR SURGICAL PROCEDURE
The procedure involves placing two cosmetic incisions in front of the ear and below the jawline. If repositioning of the upper jaw and chin is performed, those are done from an intraoral approach. Patients will either have braces in place prior to the procedure, or have temporary fixation screws placed above and below the teeth to align the jaws prior to prosthesis placement. Our incisions are normally closed with surgical glue, without the need for suture removal. Screws are removed in the office under local anesthesia.
For those patients having multiple previous surgeries or ankylosis, Dr. Sultan may place abdominal fat taken from a small incision below the belly button. This technique has been shown to reduce the formation of heterotopic bone, a postoperative condition requiring revision surgery.
Surgery is done either as outpatient or inpatient with general anesthesia.
TREATMENT OF IDIOPATHIC CONDYLAR RESORPTION/ OBSTRUCTIVE SLEEP APNEA
Combined TJR/Orthognathic Surgery
Idiopathic condylar resorption (ICR) is a relatively uncommon condition, resulting in severe skeletal jaw deformities, chronic pain and airway obstruction. Obstructive sleep apnea syndrome (OSAS) has similar associated jaw deformities. Other indications for combined surgery include orthognathic surgery revisions and severe asymmetry.
Although management of both ICR and OSAS have medical/non-surgical treatment options, an accepted method for surgically managing both conditions involve:
- Right and left TJR
- Repositioning of the upper jaw with alteration of occlusal plane
- Advancement of the upper and lower jaws
- Chin advancement with/without genioglossus advancement
ICR CASE STUDY:
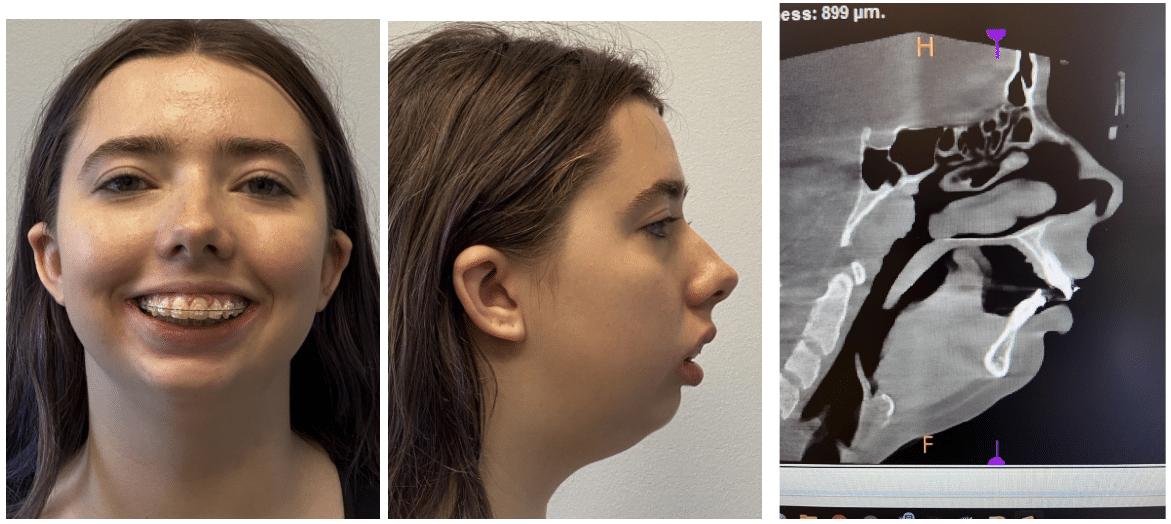
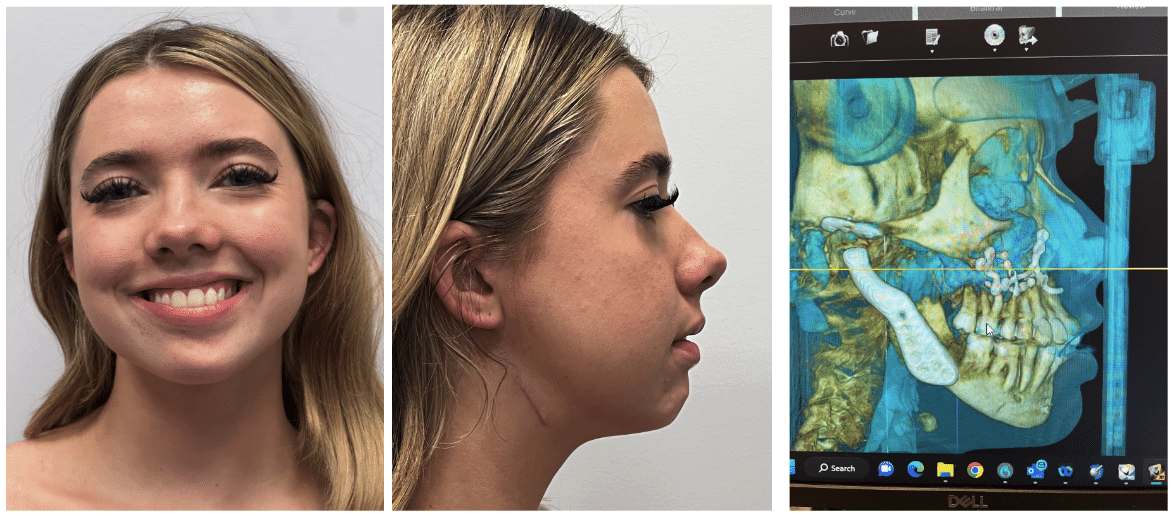
These procedures are performed for functional improvement, but offer positive esthetic changes to most patients. Planning is complex and involves thorough understanding of both TJR and orthognathic surgery.
Dr. Sultan has been specially trained in the use of total joint replacements and orthognathic surgery. He has taken part in educational meetings and performed surgery both nationally and abroad. He is one of the few surgeons in Florida and the southeast US experienced to perform these types of TMJ treatments.
PRE AND POSTOPERATIVE CARE
Dr. Sultan and his surgical staff take pride in educating their patients on preparation and care before and after their procedures. Patients and their caregivers are vital components of the surgical team. We support our care by supplying patient aids to improve and promote postoperative care.
Patients are fully advised as to their responsibilities in their own care, including:
- Understanding of the procedure and expectations
- Diet
- Exercise
- Medications
- Use of orthotic
- Physical therapy
- Activities of daily living
Dr. Sultan is always personally available 24/7 for any issues or questions that may arise.
FINISHING TREATMENT
Once patients have completed their surgical care and postoperative healing, they may require long term stabilization of their condition, which may include:
- Orthodontics
- Restorative dentistry
- Orthognathic surgery
- Use of night-time bruxism appliance
- Physical therapy
Frequently Asked Questions
Is surgery considered aggressive for TMD?
- TMJ surgery and replacement is an accepted treatment option for primary and secondary conditions when non-surgical options are limited success
- TMJ surgery is irreversible. However, some forms of non-surgical therapy can have negative, irreversible effects
- When considering surgery, both the risks and benefits of the procedure should be considered and discussed.
Posterior open bite caused by long term splint usage
Insurance coverage
- Treatment of TMD is normally covered on medical insurance
- All procedures receive prior insurance approval
- Please contact our office to determine whether we are providers for your insurance
Consultation
- Please bring all of your previous treatment records with you to your visit
Out of Town Patients:
- We see many patients who travel to our practice
- We will coordinate your visit to include consults with any other necessary providers and/or imaging studies
- We can also assist in travel and lodging arrangements for your stay
Dr. Sultan has been specially trained in the use of both partial and total joint replacements. He has taken part in educational meetings and performed surgery both nationally and abroad. He is one of the few surgeons in South Florida experienced to perform types of TMJ treatments in Ft Lauderdale, FL.
Contact us today to learn more about TMJ Treatment where Dr. Sultan is proud to treat patients from Fort Lauderdale, Pompano Beach, Boca Raton, Hollywood, and the surrounding areas.